

Arthritis often affects the hip and knee joints.
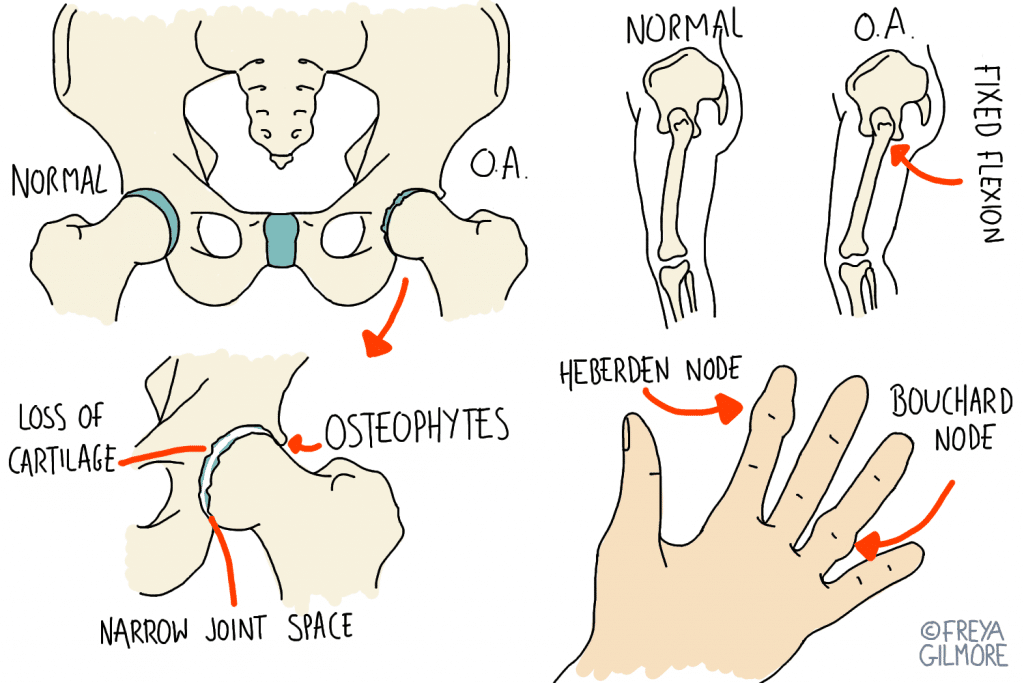
Osteoarthritis is the wear, tear, and repair process on cartilage.
So although the body tries to protect itself, it actually allows the arthritis to develop further. This is not a prognosis that needs to continue: your osteopath can help.
The knee is actually made of three joints:
Any of the three can develop arthritis. It can be particularly easy to spot when it affects the joint behind the knee cap.
Knees are normally quite crunchy joints, but this is more obvious in an arthritic knee. A healthy crunchy knee might make noise but it won’t catch or feel stiff on movement.
To try and protect the knee, the body might tighten the quadriceps muscles. Again, that isn’t really helpful. The quadriceps attach to the knee cap, so when they get tight they pull on the joint they want to protect. This can cause more pain and change the way a person moves. The cycle of restriction and poor joint health continues.
Fortunately, this joint is really responsive to osteopathic treatment. If you have arthritic knees, you might be able to see progress from the first appointment.
When osteoarthritis develops in the hip, it can lead to a total change in posture. Typically it affects the back of the joint first, and the body might react to this before you’re conscious of any problem. In order to prevent pain, the body avoids taking the hip back as far as it can. This means strides should be shorter when walking, for example, because the leg doesn’t go back as far as it used to.
But the body is clever and it finds a way around this problem. The solution is The Elderly Posture.
If you bend slightly forward at the hip, you can take steps the same length as normal but without that painful extension. You go further into flexion than you normally would, but don’t have to go past neutral when it comes to extension! To avoid falling over, the body has to compensate higher up. This could mean leaning back through the spine, or sometimes just lifting the head through the neck.
But of course there are side effects to this, apart from suddenly moving like you’re 20 years older. Failure to move through the arthritic part of the joint means failure to bring nutrition to where it is needed most. The joint continues to develop arthritis until movement does become painful. Load is also redistributed through the areas that are compensating. Holding your head up all day is hard work, and the neck is not designed for it.
If you’re already at this point, osteopathy can help, but prevention is better than cure. Catch the arthritis early and you’ll be in a much better position, literally and figuratively! Contrary to popular belief, osteoarthritis can be managed before the need for a joint replacement.
Address your arthritis as soon as you spot it. Book an appointment today.