Mythbusting in Osteopathy
We hear a lot of misinformation in clinic, whether our patients pick it up from other medical professionals or less trustworthy sources. It might seem pedantic, but correcting the way we think can hugely improve our pain. If you believe that your back is fragile, you are likely to worry more about it and become over protective. In reality, movement is exactly what most problems need. Here are some of the most common myths we hear from our patients, and the associated truths:
“Arthritis means suffering until a joint replacement”
Osteoarthritis (the “wear and tear” form of arthritis), is a condition affecting cartilage. Sometimes we forget that cartilage (and bone, in fact) are living tissues. If you broke a bone, you would expect it to heal. If your cartilage is damaged, it will take a while, but it does have the capacity to improve. Identifying arthritis in its early stages has a good outlook. The condition produces a vicious cycle, where reduced movement negatively impacts joint health overall, allowing the cartilage to become more damaged. Your osteopath can work with you to improve local movement, which allows nutrients back into the area and gives the cartilage the best chance to heal.
“A slipped disc will cause me sciatica forever”
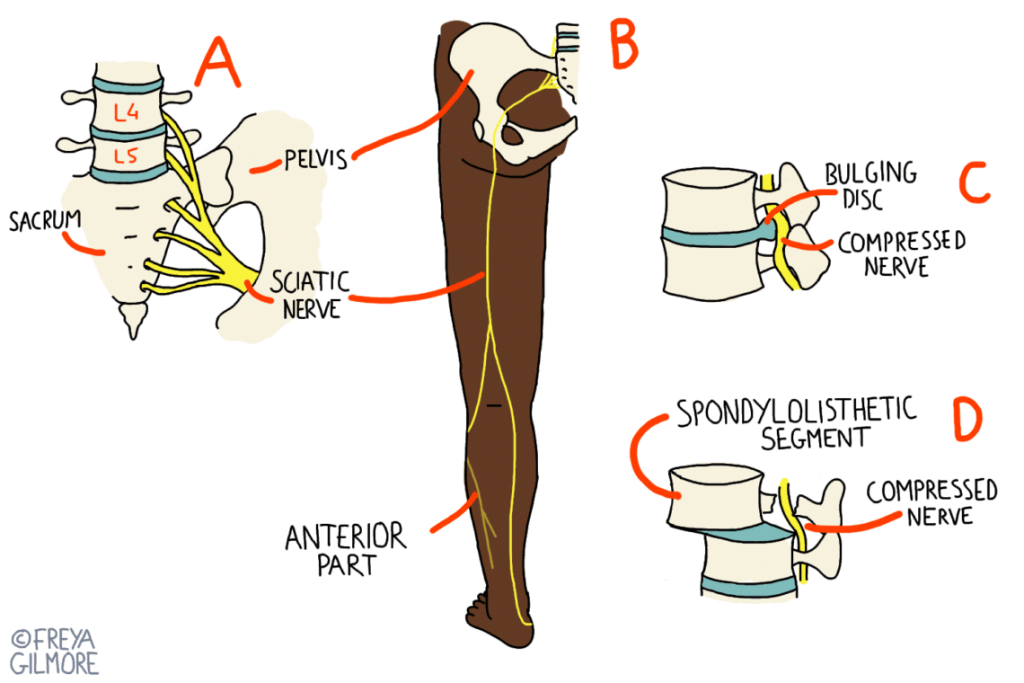
Firstly, we need to address the “slipped disc” idea. Some people use the term without thinking too much into it, but others report feeling that something popped out, or even feeling the bulge itself. Discs are made of a couple of layers: inside they are soft, whereas the outside is a flexible but strong fibrous layer. They are so firmly stuck to the vertebrae above and below, that in a severe accident, the bone is more likely to break than for the disc to detach. So don’t worry about a disc moving freely away from the spine.
What can happen is that the soft inner layer can push against a weakened spot in the fibrous layer. This can cause a bulge in the disc, or sometimes the soft layer can partially leak out. Sometimes either of these scenarios will cause pain locally in the back, or they might irritate a nerve, causing pain down the leg.
It is important to note that disc bulges often happen without any symptoms. A study showed that after the age of 40, most people had at least one bulging disc. However, less than half the population suffer from lower back pain or sciatica. This is one reason why the NHS does not routinely offer imaging for lower back pain or sciatica. This changes if there are any red flags present.
“My spine needs clicking back into place”
This one is similar to the idea of discs being somewhere they shouldn’t. Clicking a spinal joint is quite a lot like clicking your knuckles. If you’ve done so, you might notice that when you get the click, your finger moves a bit further with the noise. That’s not to say that the joint was out of place, it was just stiff.
When we click a spinal joint, we choose a restricted one. The short but powerful movement demands a little bit extra from that joint, and aims to get the movement back that has been lost. It’s never about repositioning. Rarely, a vertebra is out of place, but clicking would not be a solution. This is called a listhesis (fig. D), and is also known as a spondylolisthesis (spinal listhesis) or retrolisthesis (a backwards slippage instead of forwards). Sometimes this is purely anatomical, causing you no problems and only identified on a scan that’s looking for something else. Alternatively, it can be traumatic, in which a fracture to part of the spinal bone allows a shift in positioning. If the slip is significant enough, your osteopath may be able to feel a “step” in your spine, however this will require referral back to your GP, as we don’t click joints back into place.

